
This article was originally published on Linked In
Rippl was founded to transform dementia care: delivering the right care, at the right time, from the right people. As Chief Medical Officer, I spend much of my days making sure Rippl care teams are made up of those “right people” and that they are well taken care of once they are here. Every Rippl Changemaker is, of course, extremely capable, credentialed and, possibly more importantly, driven by a deep passion for improving the lives of seniors, particularly those living with dementia. Truly the best of the best. But dementia specialists are exceedingly difficult to find. The hard truth is that our medical education system has left the elderly behind. Consider these facts:
- Fewer than 1% of all physicians are board certified Gerontologists [American Geriatrics Society]
- Although gerontology certification takes an additional year of costly education, it results in 16% LOWER median salaries than their internist counterparts [AAMC Faculty Salary Report]
- Only 3% of licensed psychologists in the United States identify professional geropsychology as their primary or secondary specialty [American Psychological Association]
- Of the 125 to 150 geriatric psychiatry fellowship training slots nationwide, less than half of them are filled. For context, there are over 40K total psychiatry residencies offered each year – 150 is less than 1% of that! [National Institute of Health]
- By 2030, approximately 8.5 million people in the United States will be living with Alzheimer’s disease or other forms of dementia. Despite this growing number, it is estimated that the US healthcare system will only be adequately prepared to treat a small portion of them. According to the Alzheimer’s Research Foundation, around 60% of healthcare workers believe that the current system is not effectively helping patients and their families navigate dementia care even today.
With all of that in mind, we knew our mission had to go beyond the goal of filling a colossal care gap – we needed to lead the charge in building dementia-capable care teams. Rippl had to be a workforce transformation company just as much as a healthcare delivery company.
Rewind to when Rippl was not yet a company but merely an idea. Our founders knew seniors deserved better and sought out experts to uncover what proven models of dementia care existed. Of course the first stop was Harvard’s McLean Hospital who has set the standard for mental health treatment and research. No medical institution in the country knows neurocognitive disease better and the McLean team’s deep expertise in developing new and innovative approaches is unmatched. This visit sparked a meeting of the minds, ultimately leading to a deep partnership and the launch of Rippl Academy powered by McLean Hospital. This first-of-its-kind training program was built to dramatically expand the number of licensed and dementia specialty trained clinicians and close the giant expertise gap in the US.
Just last month we held our fourth collaborative workshop where Marie Clouqueur, LICSW, and Ipsit Vahia, MD – both celebrated dementia care experts from McLean – shared their knowledge with everyone from our newest care navigators to our most seasoned nurse practitioners and medical directors. This unique opportunity afforded to Rippl Changemakers is just one of the many ways we deliver on our commitment to bring the best training and resources to our team of specialists, day in and day out.
Sometimes data showing the inaccessibility of quality dementia care can be overwhelming. Yet, as the work we do at the Rippl Academy touches more and more lives, I have to say that there is so much to be optimistic and hopeful about.
#1 The tide is turning on the lack of payment models

Low levels of support and expertise in dementia can often be traced back to the lack of reimbursements for delivering this type of care. Limited revenue opportunities create a domino effect, resulting in the dramatic care gaps we see in dementia today.
But that is changing thanks to a groundbreaking new program from the Centers for Medicare & Medicaid Services (CMS) that launched July 1st. “Guiding an Improved Dementia Experience (GUIDE)” is a new Medicare alternative payment model designed to support people living with dementia and their caregivers. This model delivers on a promise in the Biden Administration’s Executive Order on Increasing Access to High-Quality Care and Supporting Caregivers and aligns with the National Plan to Address Alzheimer’s Disease. This has been a long time coming but it’s here and it’s a game changer.
#2 Care Navigators are a big unlock
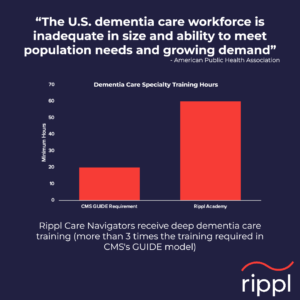 Care navigation offers a feasible model to train unlicensed people to deliver support at a larger-scale for the growing population of adults living with dementia and their caregivers. I’ve seen with my own eyes the profound difference a Care Navigator can make. In fact, care navigators are proven to reduce barriers to care but many lack the dementia care expertise needed to help patients and their caregivers manage this complex condition. This underscores why we launched the Rippl Academy. Rippl Care Navigators receive over 55 hours of dementia-specific training including our exclusive Dementia Care Foundations developed and delivered in partnership with McLean Hospital. CMS’s GUIDE model is centered on the work Care Navigators do such as care planning to prepare for the future, care coordination, and access to community resources. The Guide Model has established basic guidelines for dementia care navigation training – at Rippl we go above and beyond their requirements by a factor of 3!!
Care navigation offers a feasible model to train unlicensed people to deliver support at a larger-scale for the growing population of adults living with dementia and their caregivers. I’ve seen with my own eyes the profound difference a Care Navigator can make. In fact, care navigators are proven to reduce barriers to care but many lack the dementia care expertise needed to help patients and their caregivers manage this complex condition. This underscores why we launched the Rippl Academy. Rippl Care Navigators receive over 55 hours of dementia-specific training including our exclusive Dementia Care Foundations developed and delivered in partnership with McLean Hospital. CMS’s GUIDE model is centered on the work Care Navigators do such as care planning to prepare for the future, care coordination, and access to community resources. The Guide Model has established basic guidelines for dementia care navigation training – at Rippl we go above and beyond their requirements by a factor of 3!!
#3 We’re creating the new gold standard in holistic dementia care training
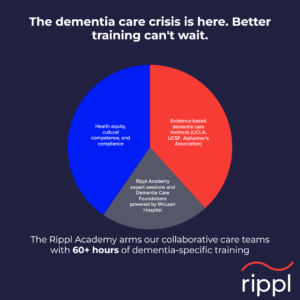 Globally, clinicians are both under-educated on dementia, and under-resourced to provide adequate post-diagnosis care for people living with dementia. Medical schools and other training programs focus on the medical interventions of an illness rather than psychosocial challenges for patients and their families. For people living with dementia and their caregivers, this just doesn’t cut it. Care teams must become dementia care specialists and be skilled in the critical areas that help people navigate the day to day while also preparing for the future. This is why we built the Rippl Academy – exclusively for our care teams. At the academy, we focus on the medical condition of dementia but also dig deep into behavioral health issues, social determinants of health, stigma of dementia, challenges of family dynamics, relationship building and more. Academy sessions range from the Foundations in Dementia training program developed with McLean Hospital, health equity training from our partners at Violet, as well as a number of specialized experiences like a recent motivational interviewing clinic. It all works together as we endeavor to set the gold standard and build a skilled, dementia-capable workforce.
Globally, clinicians are both under-educated on dementia, and under-resourced to provide adequate post-diagnosis care for people living with dementia. Medical schools and other training programs focus on the medical interventions of an illness rather than psychosocial challenges for patients and their families. For people living with dementia and their caregivers, this just doesn’t cut it. Care teams must become dementia care specialists and be skilled in the critical areas that help people navigate the day to day while also preparing for the future. This is why we built the Rippl Academy – exclusively for our care teams. At the academy, we focus on the medical condition of dementia but also dig deep into behavioral health issues, social determinants of health, stigma of dementia, challenges of family dynamics, relationship building and more. Academy sessions range from the Foundations in Dementia training program developed with McLean Hospital, health equity training from our partners at Violet, as well as a number of specialized experiences like a recent motivational interviewing clinic. It all works together as we endeavor to set the gold standard and build a skilled, dementia-capable workforce.
Looking to the future
One of Rippl’s core values is Care Team Obsession, which simply means if we take good care of our care teams, they will take excellent care of the people that we serve. This doesn’t just require a great culture or good benefits – it’s about arming and preparing Team Rippl to provide tailored care to each patient and caregiver based on their unique situation. That requires specialized, ongoing training and we are committed to continuously evolving Rippl Academy to deliver on that promise. I hope you join me in my optimism about the future of dementia care. As we like to say at Rippl, “if not us, then who?” Let’s do this.
Jamie Sharp, MD is Rippl’s Chief Medical Officer








