
This article was originally published on Linked In
Throughout my career, I’ve repeatedly heard the mantra “technology will fix healthcare,” be it the internet, electronic health records, or mobile devices. I’ve also witnessed the original triple aims for US healthcare innovation — Patient Experience, Population Health, and Cost — expand to include Care Team Well-Being and Health Equity. Yet our system continues to be plagued with mediocre outcomes, rising costs, clinician burnout, and a persistent failure to serve those most in need.
Now, as if out of the blue, Large Language Models and AI have become the newest, shiny objects guaranteed to fix what ails the healthcare system. It’s easy to be skeptical based on past experience with so-called silver bullets. But, this time may be different. Healthcare is the industry with the greatest potential for transformation by modern AI, especially in the United States where our per-capita healthcare expenditure is double the G7 average and our outcomes are arguably the worst of the group. If used correctly, AI will:
- Save money by automating costly administrative tasks like documenting patient encounters and obtaining insurance preauthorizations
- Improve health outcomes by giving clinicians more time and space to focus on each individual patient with the support of intelligent tools
- Increase access and equity in our healthcare system by enabling 24×7 communication services that are fluent in the dozen plus languages commonly used across the country.
Human-driven, AI-powered
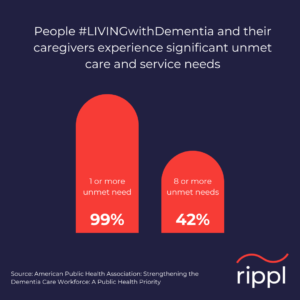
Nowhere is this more true than in Dementia Care where we are barely scratching the surface of what can be achieved through better care management and caregiver support. Today, the unmet needs for this group are countless and often catastrophic. Here at Rippl we are making deep investments in AI innovation to improve Dementia Care Management, which is ideally suited for the transformations outlined above. Dementia Care Management is unique amongst healthcare disciplines in the need to engage not just an interdisciplinary team of clinicians, such as physicians, nurse practitioners, and social workers, but also the patient’s primary caregiver, typically a family member or friend who shoulders an enormous burden in a labor of love. Our care model is orchestrated by a highly trained and dedicated group of Care Navigators who provide consistent support to our patient families and act as connectors to the rest of our clinicians as well as the patient’s local medical providers. Their tasks are as varied as the day is long: teaching our families about the intricacies of Alzheimer’s and all other dementias, finding local community resources and benefits, navigating complex health systems, and most of all being a trusted, empathetic companion on what can be an incredibly difficult journey.
 That trusted human relationship is at the heart of our care model. Not only is Alzheimer’s the most expensive disease in the country, it is also one of the least understood and discussed. Our care navigators deeply understand the extreme difficulties our families face and are continually educating, facilitating, and guiding them through the long journey of the disease. But with such a broad and complex workload, it’s a gigantic challenge for our navigators to balance the administrative tasks of their job with actually supporting and assisting our families. As AI capabilities continue to expand from managing and processing vast pools of information to gaining greater powers of autonomous two-way communication, we have an unprecedented opportunity to redefine care management, paradoxically making it more human.
That trusted human relationship is at the heart of our care model. Not only is Alzheimer’s the most expensive disease in the country, it is also one of the least understood and discussed. Our care navigators deeply understand the extreme difficulties our families face and are continually educating, facilitating, and guiding them through the long journey of the disease. But with such a broad and complex workload, it’s a gigantic challenge for our navigators to balance the administrative tasks of their job with actually supporting and assisting our families. As AI capabilities continue to expand from managing and processing vast pools of information to gaining greater powers of autonomous two-way communication, we have an unprecedented opportunity to redefine care management, paradoxically making it more human.
AI + Dementia Care = increased access
My personal mission at Rippl is to harness these new generations of AI in support of our navigators and clinicians to amplify their skills and effectiveness and scale their work to the millions of families in need. Our focus is on the center of this venn diagram, identifying useful tasks that LLMs can do well and that people generally can’t or don’t want to do.
Things like listening to endless hours of phone conversations to accurately pluck out key details for patient records, scouring through dozens of arcane government websites to understand a family’s eligibility for community benefits, or meticulously reviewing every single patient’s case on a daily basis to find the best next helpful action. By offloading these tasks, we free our navigators and clinicians to focus their attention exclusively on their patients and families.
Additionally, we will be able to take advantage of AI’s extraordinary multilingual and multi-cultural capabilities to allow our care team to communicate with families in their native languages and idioms. Engaging with every community, regardless of language abilities, geography, and technology proficiency is vital to our goal of reaching every dementia affected family who can benefit from our services.
The future is now
From “2001: A Space Odyssey” to “Star Wars” to “Iron Man,” talking computers were futuristic sci-fi inventions that seemed forever out of reach. We long ago invented flying cars (turns out they aren’t very practical), cloning (do you really want a baby who’s your twin?), and brain implants (ouch!), and we even survived a global pandemic. It’s easy to appreciate both extremes of hyperbole and skepticism surrounding AI, but the fact remains that a stunning aspect of our sci-fi future has become our present reality: computers can now process vast oceans of information and fluently converse with us about it. This power alone will not fix the US healthcare system, but it will go a long way to amplifying the skills, knowledge, effectiveness, and accessibility of the humans on the front line.
Joe Chung is Rippl’s CTO and Head of AI








