
This article was originally published on Linked In
Fact: our healthcare system has, by and large, been letting dementia patients and their caregivers down. The reality is that it’s built for acute, intermittent care, and dementia just doesn’t fit that framework. Typically with a new diagnosis, whether it’s heart disease or a broken arm, you have a predetermined sequence of treatments and follow up care. The care plan for these acute illnesses is carved out in our healthcare system. Sadly, we are behind in setting up that framework to support people with dementia.
All too often families are left to navigate this complicated disease on their own. Along with a dementia diagnosis, they are often handed the Alzheimer’s Association care line to call and not much else. By virtue of being the only accessible, trustworthy source of information post diagnosis, most doctors send people to the Alzheimer’s Association and hope everything goes well until their next visit. How crazy is it that our healthcare system relies heavily on philanthropy to take care of the millions of people diagnosed with dementia? We must do better for our seniors.
The good news is that innovative, evidence-based programs, like UCSF’s Care Ecosystem, have shown collaborative, longitudinal care improves the quality of life for people with dementia and their caregivers. [1] The bad news is that this care can be hard to find. [2]
As the prevalence of dementia sharply rises with aging baby boomers, millions of patients and their caregivers will continue to seek out help within a system that is unprepared to respond. We need to build and deliver new care models that address the harsh reality of this devastating disease. At scale. But how do we get there?
#1 – Interdisciplinary care teams providing the right kind of care
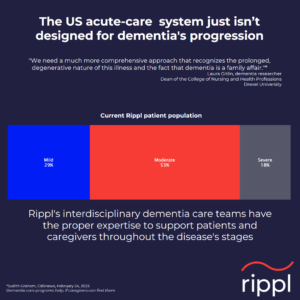 Our healthcare system defers to intense medical interventions for most conditions rather than focusing on the care that caregivers and people with dementia needand want. What’s really needed are interdisciplinary teams focused on listening, empathizing and connecting with people that are struggling through the stages of dementia. Psychosocial support, education and filling gaps in resources will improve the lives of patients and their caregivers while also promoting appropriate utilization.
Our healthcare system defers to intense medical interventions for most conditions rather than focusing on the care that caregivers and people with dementia needand want. What’s really needed are interdisciplinary teams focused on listening, empathizing and connecting with people that are struggling through the stages of dementia. Psychosocial support, education and filling gaps in resources will improve the lives of patients and their caregivers while also promoting appropriate utilization.
At Rippl, our dementia trained interdisciplinary teams are made up of nurse practitioners, licensed clinical social workers, and care navigators who work collaboratively to continually assess the needs of the patient and the caregiver and deliver care appropriate for the time and situation. The care team is in it for the long haul to maintain continuity, allow ongoing touchpoints as issues arise and prepare the caregiver for the future stages of the disease.
While the entire team remains engaged throughout the progression, each stage requires different expertise and care to flex up. For example, in the early stages, the support and resources care navigators provide are vital, whereas, nurse practitioners become more involved as medical complexity increases. Flexible care delivery to meet the unique needs of each patient and accessibility to a consistent care team is the answer to improving quality of life for patients and their families.
#2 – Dementia does not exist in isolation
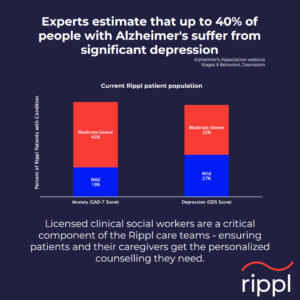 Dementia is a complex condition and is often paired with mental health disorders. Clinical research has shown that, depending on what type of dementia a patient has, 33-60% will also have depression.[3] There has always been a tight linkage between depression and dementia. In fact, recent studies show that stress and depression might be linked to an increased risk of Alzheimer’s disease. [4] These statistics support the need for dementia care teams to include licensed clinical social workers along with access to psychiatric nurse practitioners.
Dementia is a complex condition and is often paired with mental health disorders. Clinical research has shown that, depending on what type of dementia a patient has, 33-60% will also have depression.[3] There has always been a tight linkage between depression and dementia. In fact, recent studies show that stress and depression might be linked to an increased risk of Alzheimer’s disease. [4] These statistics support the need for dementia care teams to include licensed clinical social workers along with access to psychiatric nurse practitioners.
We must meet people where they are and bring the expertise and care that’s right for them. For example, many of our dementia patients experience apathy, defined as diminished motivation and emotional responsiveness, a common symptom present in dementia that can also be confused with depression. It is imperative to accurately diagnose and deliver the proper care. Our psychiatric nurse practitioners perform detailed evaluations to identify intermingled behavioral health disorders. If present, the patient will receive psychotherapy from our social workers and potentially medication interventions to improve their quality of life. Dementia is complex and requires a diverse care team with the expertise to deliver the right care.
#3 – Focus on the day-to-day
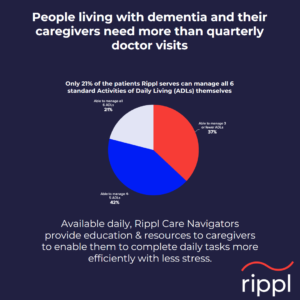 As dementia progresses, simple daily tasks become overwhelming for the patient. Brushing one’s teeth, dressing and other activities of daily living (ADLs) become difficult due tochanges in brain function. The sequence of events to complete a task becomes overwhelming and creates frustration. This frustration often leads to disruptive new behaviors. For the patients we serve, 79% need some level of ADL support. Navigating the daily needs of the patient falls on the shoulders of thecaregivers who may lack an understanding of why this disconnect is occurring. Supporting basic needs of a person with dementia is physically and emotionally taxing. Burnout of our caregivers has been called a silent health crisis. The good news is that care navigators can offer suggestions and resources that can help the caregiver ease the ADL process and bring harmony to the interactions. Care navigators will explore what barriers or behaviors exist for each individual patient and bring solutions with educational materials, in-home support and group therapy. Caregiver burden can often be drastically reduced with something as simple as setting up meal delivery.
As dementia progresses, simple daily tasks become overwhelming for the patient. Brushing one’s teeth, dressing and other activities of daily living (ADLs) become difficult due tochanges in brain function. The sequence of events to complete a task becomes overwhelming and creates frustration. This frustration often leads to disruptive new behaviors. For the patients we serve, 79% need some level of ADL support. Navigating the daily needs of the patient falls on the shoulders of thecaregivers who may lack an understanding of why this disconnect is occurring. Supporting basic needs of a person with dementia is physically and emotionally taxing. Burnout of our caregivers has been called a silent health crisis. The good news is that care navigators can offer suggestions and resources that can help the caregiver ease the ADL process and bring harmony to the interactions. Care navigators will explore what barriers or behaviors exist for each individual patient and bring solutions with educational materials, in-home support and group therapy. Caregiver burden can often be drastically reduced with something as simple as setting up meal delivery.
That’s why consistent and ongoing support from a care navigator is so critically important.
Passionate About Being Part of the Solution
As a former primary care provider, I hesitated to deliver a diagnosis of dementia to my patients and their caregivers. Dementia is not a diagnosis that you can fit into a 15 minute time slot within the overburdened schedules of a primary care physician. I had no magical medical treatment to prescribe that would reverse the deterioration in mental and functional capabilities that would inevitably overcome my patient. At each visit, I, like the family, witnessed the gradual loss of the vibrant person that we all knew. I lacked a dementia trained care team that would walk alongside the patient and the family on this uncertain journey, providing much needed answers to questions and even a sense of hope. I felt ill prepared and inadequate to meet the needs of my patients and their families. They deserved better.
At Rippl, we are rising to the challenge to fill this void for patients, caregivers and lessen the demand on primary care physicians. Hearing our care navigators describe the heartwarming discussions they have with patients and caregivers reminds me why I became a physician. What we are doing is helping to bring more good days to our patients and their families. Rippl is making a difference and I am honored to be part of this noble mission.
Dr. Jamie Sharp, Changemaker and Chief Medical Officer at Rippl
Sources:
[2] Improving Outcomes for Individuals Living with Dementia
[3] Depression in dementia with Lewy bodies: A comparison with Alzheimer’s disease, Neuropsychiatric aspects of multi-infarct dementia and dementia of the Alzheimer type, The prevalence of depressive symptoms in frontotemporal dementia: a meta-analysis
[5] Activities of Daily Living – StatPearls – NCBI Bookshelf








